Case report: PANDAS and persistent Lyme disease with neuropsychiatric symptoms
Complete resolution of symptoms following IVIg and antimicrobial treatment
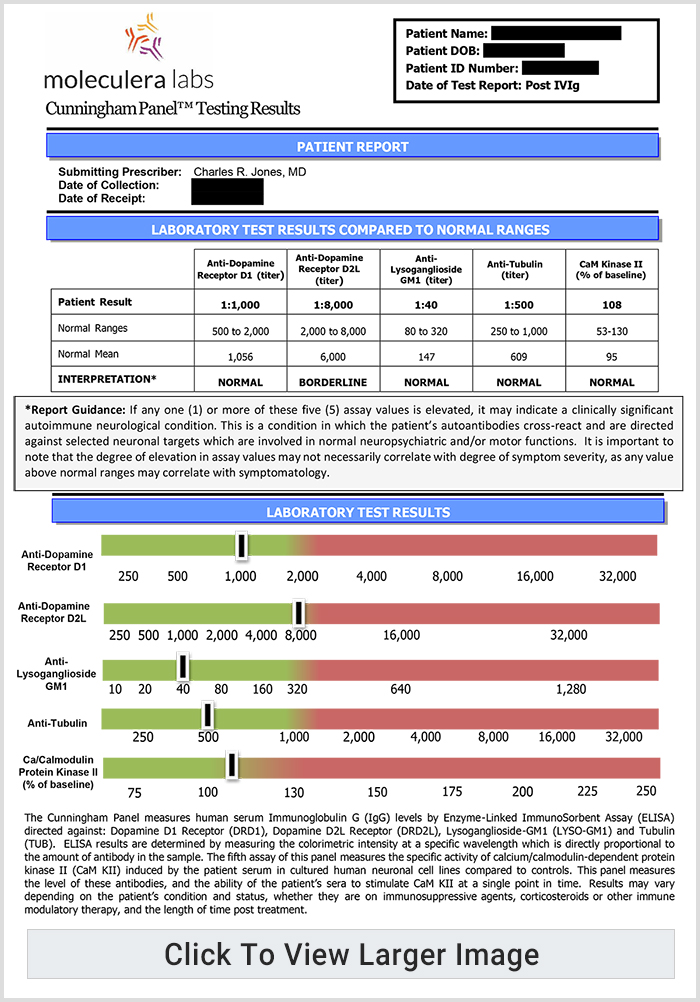
In this newly published article, the authors describe the diagnosis, symptom progression and treatment of a 7-year-old female with serological evidence of Lyme disease who developed multiple neuropsychiatric symptoms six months after visiting a tick endemic region.1 Prior to her diagnosis of Lyme disease, the patient had been treated for three distinct episodes of streptococcal pharyngitis and diagnosed with PANDAS (Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcal infections).
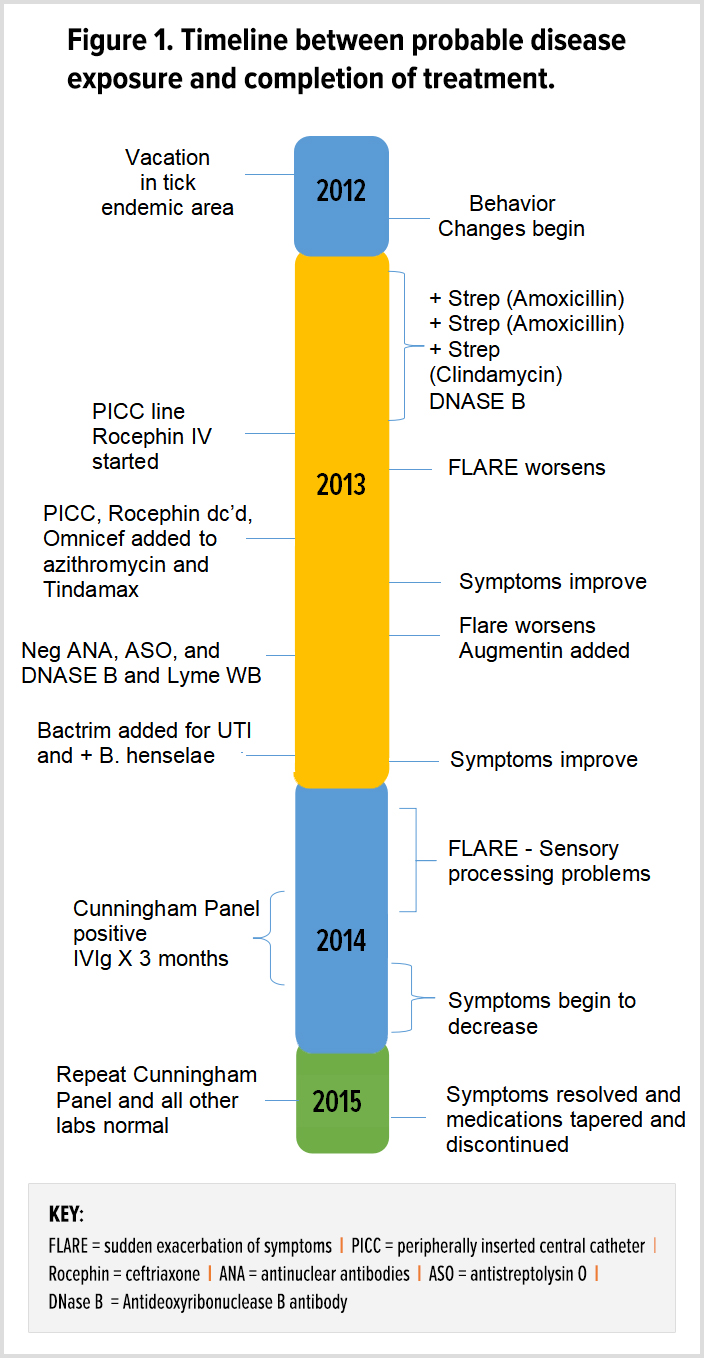
Over a three-week period, the patient developed multiple symptoms including obsessions, compulsions, aggressive behavior, dramatic declines in cognitive functioning, loss of math skills, the onset of dysgraphia and difficulty with social cues, fatigue, nighttime awakening, chills, joint and muscle pain, moodiness, separation anxiety and panic attacks.
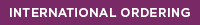
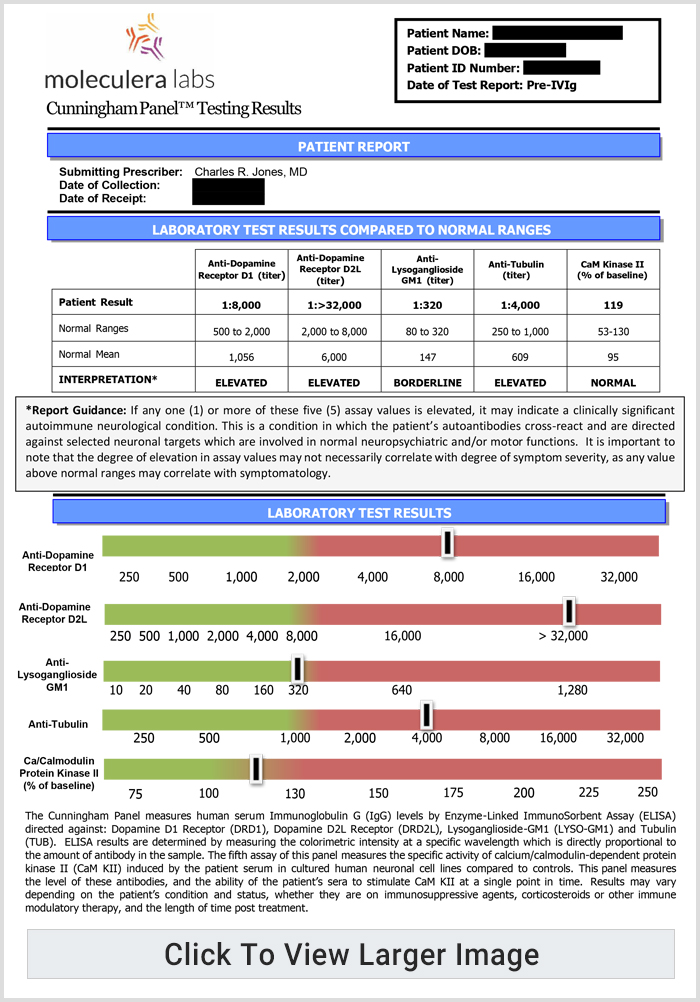
Following several months of oral and IV antimicrobial treatment, the Cunningham Panel™ of tests was ordered to assess the presence of antineuronal antibodies against specific neuronal receptors. Based upon test results, “the decision was made to prescribe intravenous immunoglobulin (IVIg) in accordance with established treatment guidelines for the patient’s level of symptom severity.”
“Over a span of 31 consecutive months of treatment with various antimicrobials and 3 courses of intravenous immunoglobulins (IVIg), she experienced complete remission and remains symptom free at the time of this publication.”
The authors conclude that “This patient’s case may be representative of numerous other cases of autoimmune neuropsychiatric illnesses where a patient may have concomitant infections and co-morbid diagnoses.”
“As evidenced by her recovery and resolution of symptoms, treating both the Lyme infection and streptococcal infection, as well as treating the underlying autoimmune etiology of her neuropsychiatric symptoms resulted in a successful outcome.”
- “Patients with chronic neuropsychiatric symptoms who do not respond adequately to traditional psychotropic medications may have an underlying immune-mediated condition triggered by one or more infections as evidenced in this case report.”
- “Improvement in neuropsychiatric symptoms does not typically occur unless all co-infections are addressed and resolved,” according to the treating physician’s clinical experience.
- “The presence of elevated antineuronal antibodies identified by the Cunningham Panel™ provided an aid in diagnosis and in directing immunomodulatory treatment.”
- “The post-treatment resolution of these autoantibodies provided pathophysiological support for addressing both the infection(s) and the underlying immune system dysfunction which resulted in a positive medical outcome for this patient.”
- “There is increasing evidence that IVIg and immunoglobulins are effective in treating autoimmune neuropsychiatric illness although the mechanism of action is uncertain.”
Digital Information Packet
To learn more about infection-triggered basal ganglia encephalitis syndromes, such as PANS/PANDAS, view our online informational packet. We have compiled journal articles and video clips that may be helpful to you.
Additional Research
Lyme Disease and the Immune System: Elevated Neuronal Autoantibodies Associated with Persistent Symptoms
Cunningham Panel™ results indicate Lyme disease may trigger autoimmune dysfunction
Study Demonstrates Clinical Value of the Cunningham Panel™ and Accuracy in Patients with Symptoms of an Autoimmune Encephalopathy
Antineuronal antibodies correlate with pre- and post-treatment neuropsychiatric symptoms
Autoantibody Biomarkers for Basal Ganglia Encephalitis in Sydenham Chorea and Pediatric Autoimmune Neuropsychiatric Disorder Associated With Streptococcal Infections
Clinicians: Schedule a Personal Phone Consultation with our Clinical Staff
Learn more about how the Cunningham Panel™ of tests can assist you in diagnosing treatable autoimmune encephalopathies characterized by abnormal neuropsychiatric behaviors. Schedule your personal phone consultation with a Moleculera Labs clinical staff member by completing the form below.
- Case Report: PANDAS and Persistent Lyme Disease With Neuropsychiatric Symptoms: Treatment, Resolution, and Recovery. Cross A., Bouboulis D., Shimasaki C., Jones C.R. Front. Psychiatry, 02 February 2021 | https://doi.org/10.3389/fpsyt.2021.505941